Last summer I wrote about the challenges of vaccine development in relation to the COVID-19 pandemic. At that time it was predicted that a vaccine might be available as early as January 2021. During fall term I taught Clinical Microbiology and the pandemic came up numerous times. The impact that this pandemic has had on each of us created immediate and personal connections to course content: wearing masks, learning online, COVID-19 testing, quarantine... The topics of vaccines and herd immunity, however, struck me as the most timely; we covered these the same week that the nursing students in the course received their first dose of the COVID-19 vaccine.
We develop immunity against many of the pathogens we are exposed to throughout our lives. The first exposure to a pathogen primes our immune systems to react with more speed and force upon second exposure to the same pathogen. The benefit is significant--it reduces the chance that we will become ill. Vaccination speeds this process along, and has the added benefit of producing memory in our bodies without first producing disease.
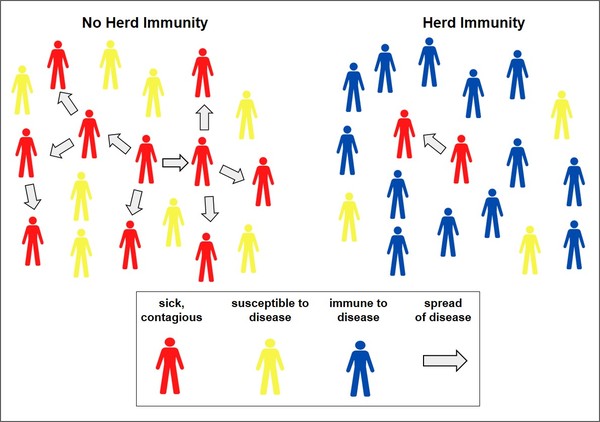
Our individual immunity also protects those around us, a phenomenon called herd immunity. When we are exposed to a pathogen our immune systems have seen before, they are more likely to destroy the pathogen before it has a chance to spread to someone else. We become a “dead end” for that pathogen, and the spread of it within our community slows down. In this way, an outbreak can be contained. For pathogens that cause severe disease, it is critical for the majority of the population to be immune so that they do not transmit the pathogen to those who have a high risk of developing severe disease. In this way, high-risk individuals can be protected by the strong immune systems of those around them.
When is herd immunity achieved? For pathogens that are contagious (spread easily from person to person) and are novel/new to a population such as SARS-CoV-2, a high percentage of the population needs to develop immunity before an outbreak can be contained. Current estimates suggest that between 70-95% of the U.S. population will need to be immune to achieve herd immunity from COVID-19. The higher percentage will likely be needed in areas with a large high-risk population or high population density. Those who have been exposed to SARS-CoV-2 and recovered (or were asymptomatic) are likely to be immune, but our experience with this virus is too recent to know yet if immunity lasts long-term. The mutation rate of this virus will also impact our ability to achieve herd immunity, since a variant strain of SARS-CoV-2 in a population may not be recognized by those who are immune to a different strain.
Vaccination, however, provides a faster and safer way to reach herd immunity. The Food and Drug Administration (FDA) approved the emergency use of both Pfizer’s and Moderna’s COVID-19 vaccines in December. As of February 26th, over 46 million in the U.S. have received at least one dose of a COVID-19 vaccine (about 14% of the population), and over 25 million have received the required 2 doses. One estimate suggests that without a vaccine, herd immunity against COVID-19 would not be achieved in the U.S. until at least May of 2025. As vaccination becomes available to the wider population, we can reduce this time frame. “Best case scenario” estimates suggest that herd immunity could be reached mid-to-late 2021. The exact time frame depends upon many factors including widespread distribution and use of the vaccine, its effectiveness at producing long-term immunity, and a low mutation rate of the virus. Each of these factors presents challenges to overcome, and it is likely that reaching herd immunity by this summer may not be realistic.
Each of us, however, can continue to limit the spread of SARS-CoV-2 in our communities through wearing masks, routine hand washing, and limiting our number of close contacts. As the opportunity to be vaccinated arises (as it did for many of my students in January), we can take another step in reducing the spread of this virus. These actions will help us return to a state of normalcy sooner while continuing to protect the most vulnerable among us. When we do our best to protect the health of not just ourselves but others during this pandemic, the community benefits as a whole. Perhaps, then, we can describe this collective aim more aptly as “community immunity.”
An Iowa College in the Liberal Arts Tradition
Developing Herd Immunity Against COVID-19
The ideas and viewpoints expressed in the posts on the Ideas and Creations blog are solely the view of the author(s). Luther College's mission statement calls us to "embrace diversity and challenge one another to learn in community," and to be "enlivened and transformed by encounters with one another, by the exchange of ideas, and by the life of faith and learning." Alumni, faculty, staff, students and friends of the college are encouraged to express their views, model "good disagreement" and engage in respectful dialogue.
By Gwen Strand, Instructor in Biology





Add a comment